June 4, 2015 - Planned neck dissection (ND) is often performed before or after patients with head and neck squamous cell carcinoma (HNSCC) undergo chemoradiotherapy (CRT) for locally advanced nodal metastases. Using PET/CT to detect persistent disease could decrease the number of NDs and possibly lead to improved patient outcomes, according to a study1 presented at the 2015 ASCO Annual Meeting.
Researchers conducted a multi-centre, randomized, phase III, controlled trial (RCT) comparing PETCT guided active surveillance with planned neck dissection (ND) for locally advanced (N2/N3) nodal metastases (LANM) in patients with head and neck squamous cell cancer (HNSCC) treated with primary radical chemoradiotherapy (CRT). The study aimed to determine the efficacy and cost-effectiveness of PET/CT-guided surveillance, compared to planned ND, in a multicentre randomised setting.
The authors concluded that PET/CT-guided active surveillance showed similar survival outcomes to ND arm, but resulted in considerably fewer NDs, and fewer complications, supporting its use in routine practice.
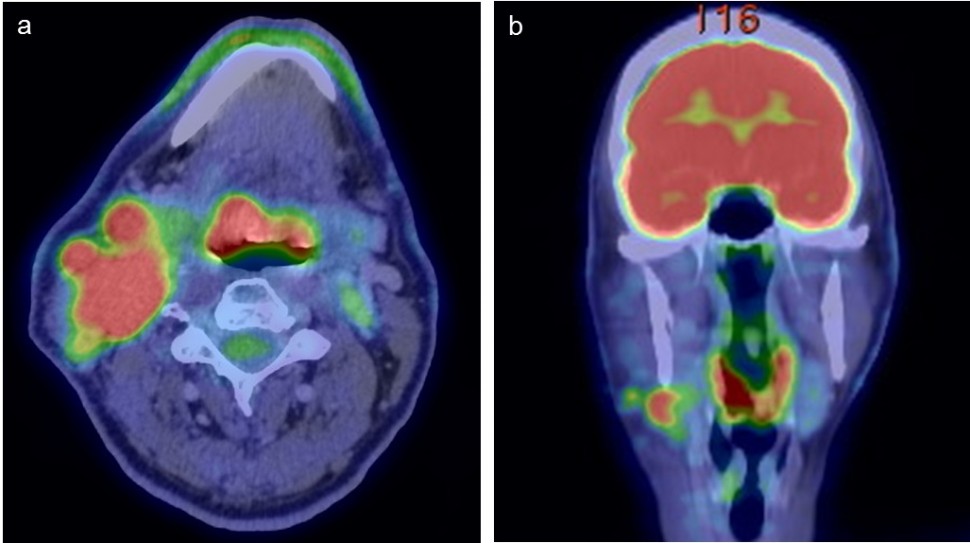
Image: PET CT avid small right tongue base primary with extensive nodal disease in right neck. References: Department of Medical Imaging, Gold Coast University Hospital, Gold Coast/ Australia 2014. Source: 10.1594/ranzcr2014/R-0171
On behalf of the PET-NECK Trial Group, Alison Florence Smith, MSc, of the University of Leeds, United Kingdom, presented results from a 2-year cost effectiveness within-trial analysis and a decision model analysis of lifetime cost effectiveness (Abstract 6010).2 When compared with ND at a £20,000 per QALY threshold, the lifetime analysis results showed that PET-CT surveillance has an 86% probability of being cost saving, a 45% probability of being more effective, and a 50% probability of being cost effective. The author noted that a great deal of uncertainty surrounds the long-term data because the lifetime decision model is substantially extrapolated beyond the 2-year trial period.
“These important data combined with large contemporary institutional series reporting excellent outcomes with response-based neck management strongly suggest response-based neck management should be the standard of care for patients with N2/3 selected to undergo radiation plus or minus chemotherapy,” said Discussant John N. Waldron, MD, of the University of Toronto, Canada.2
1. Mehanna HM, Wong WL, McConkey CC, et al A multi-centre, randomized, phase III, controlled trial (RCT) comparing PETCT guided active surveillance with planned neck dissection (ND) for locally advanced (N2/N3) nodal metastases (LANM) in patients with head and neck squamous cell cancer (HNSCC) treated with primary radical chemoradiotherapy (CRT). J Clin Oncol 33, 2015 (suppl; abstr 6009). 2015 ASCO Annual Meeting.
2. PET-CT Surveillance for HNSCC Demonstrates Noninferior Outcomes, Lower Costs. ASCO Virtual Meeting Website. http://am.asco.org/pet-ct-surveillance-hnscc-demonstrates-noninferior-outcomes-lower-costs.




