April 8, 2015 - A 40% rate of discordance between surgical and post-operative computed tomography (CT) assessments of residual disease in patients treated for advanced ovarian cancer (stage III/IV) had a significant impact on the risk of ovarian cancer progression.1
It’s not the first time a study has shown a large discordance ratio between surgeon and CT assessment after cytoreduction,2 but in this recent study, presented at the 46th Annual Meeting of the Society of Gynecologic Oncology held on March 28-31, 2015, the disparity showed a negative affect on progression-free survival (PFS) or overall survival (OS).
Ramez N. Eskander, MD, a UC Irvine Health surgeon, and colleagues retrospectively reviewed 1,091 cases from the Gynecologic Oncology Group 218 trial, which compared postoperative platinum-taxane chemotherapy with or without bevacizumab (Avastin) in patients with newly diagnosed, advanced ovarian cancer. They defined optimal surgical debulking as <1 cm of residual disease. The findgins showed CT identified at least one target lesion ≥1 cm in 251 cases. In the subgroup of patients with residual disease, more than half had three or more measurable lesions on the baseline CT scan.
Discordant lesions were associated with a PFS hazard ratio of 1.30. Patients who had no discordant lesions and no lesion on the postoperative CT scan had a median PFS of 18.3 months, whereas patients with discordant lesions had a median PFS of 12.8 months. OS was similar between patients with and without discordant lesions, associated with an HR of 0.994.
Dr. Eskander was awarded the 2015 Presidential Award from the Society of Gynecologic Oncology for his findings about surgeons' assessment of residual cancer following ovarian cancer surgery at the 46th Annual Meeting of the Society of Gynecologic Oncology held on March 28-31, 2015.
Eskander’s abstract, Correlation between surgeon’s assessment of residual disease and findings on postoperative pre-treatment computed tomography scan in women with advanced stage ovarian cancer reported to have undergone optimal cytoreduction: An NRG Oncology/GOG study, was selected by the members of the SGO Annual Meeting Program Committee acknowledging the presentation of scientific data that has a direct impact on the care and treatment of women’s cancers.
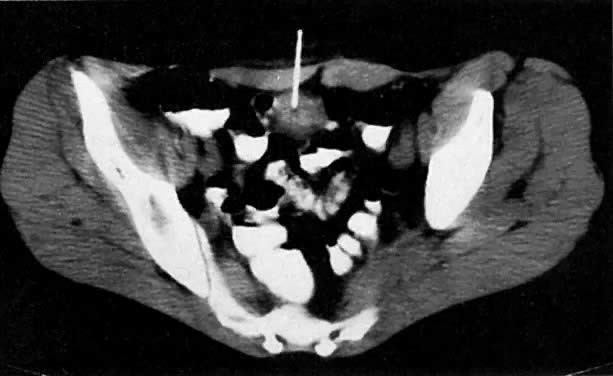
A 47-year-old woman with stage IB ovarian cancer. Axial CT scan of the pelvis shows large, bilateral cystic ovarian masses ( o ). Source: GLOWN. Abu-Yousef, M, Pelsang, R, et al, Glob. libr. women's med., (ISSN: 1756-2228) 2008; DOI 10.3843/GLOWM.10266
1. Eskander RN, et al "Correlation between surgeon's assessment of residual disease and findings on postoperative pretreatment computed tomography scan in women with advanced stage ovarian cancer reported to have undergone optimal cytoreduction: An NRG Oncology/GOG study" SGO 2015; Abstract 5.
2. Chi DS1, Ramirez PT, Teitcher JB, et al. Prospective Study of the Correlation Between Postoperative Computed Tomography Scan and Primary Surgeon Assessment in Patients With Advanced Ovarian, Tubal, and Peritoneal Carcinoma Reported to Have Undergone Primary Surgical Cytoreduction to Residual Disease 1 cm or Less. J Clin Oncol. 2007 Nov 1;25(31):4946-51.




