February 3, 2015 - The use of targeted MR/ultrasound fusion biopsy, compared with standard extended-sextant ultrasound-guided biopsy, in men undergoing biopsy for suspected prostate cancer, was associated with increased detection of high-risk prostate cancer and decreased detection of low-risk prostate cancer.1
The prospective cohort study at the National Cancer Institute was designed to assess targeted versus standard biopsy and the two approaches combined for the diagnosis of intermediate- to high-risk prostate cancer. The 1003 male participants underwent multiparametric prostate magnetic resonance imaging (MR) to identify regions of prostate cancer suspicion followed by targeted MR/ultrasound fusion biopsy and concurrent standard biopsy.
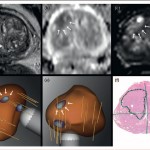
Source: Prostate MRI-Ultrasound Imaging and Biopsy (Journal of Urology Article 2013).
Targeted biopsy diagnosed 30% more high-risk cancers compared to standard biopsy (173 vs 122 cases) and 17% fewer low-risk cancers (213 vs. 258 cases). When standard biopsy cores were combined with the targeted approach, an additional 22% of patients with mostly low-risk prostate cancer were diagnosed (83% low risk, 12% intermediate risk, and 5% high risk). The predictive ability of targeted biopsy for differentiating low-risk from intermediate- and high-risk disease in 170 men with whole-gland pathology after prostatectomy was greater than that of standard biopsy or the two approaches combined.
The authors concluded that targeted MR/ultrasound fusion biopsy, compared with standard extended-sextant ultrasound-guided biopsy, was associated with increased detection of high-risk prostate cancer and decreased detection of low-risk prostate cancer.
Source:
1. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer, Mohammad Minhaj Siddiqui, et al., JAMA, doi:10.1001/jama.2014.17942, published online 27 January 2015.




